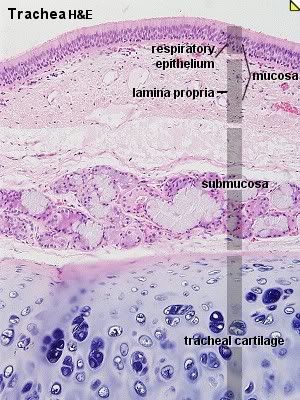
Figure 5: The trachea. (From http://www.octc.kctcs.edu/GCaplan/anat2/notes/tra11he.jpg)
The trachea is a tube supported by incomplete rings of cartilage which help to keep it patent, yet allow for stretching of the esophagus for food passage. The trachea connects the larynx to the primary bronchi [2, 6]. It is lined with ciliated pseudostratified columnar epithelium with mucus producing goblet cells and serous cells which secrete an isotonic fluid. The mucus forms a watery layer on top of the epithelium and traps inhaled particles. The cilia beat upwards and carry the debris filled mucus toward the larynx and pharynx where is it swallowed and then digested [1, 8]. The epithelium and lamina propria, consisting of loose connective tissue with elastic fibers, of the trachea are collectively referred to as the mucosa. The layer of connective tissue below the mucosa is referred to as the submucosa, and muco-serous glands in this layer supplement the secretions of the cells in the epithelium. Under the submucosa is the perichondrium [6, 8].
Bronchi and Bronchioles
The trachea divides into the left and right primary bronchi at the carina, which is a ridge in the sagittal plane of the trachea and are characterized by the presence of glands, smooth muscle, and supporting cartilage [1, 2]. They penetrate the lung at an area called the hilum. The primary bronchi undergo extensive branching within each lung, first dividing into lobar bronchi then segmental bronchi, and eventually terminate in the bronchioles, which do not have glands or catrilage and have a thick layer of smooth muscle [2, 8].
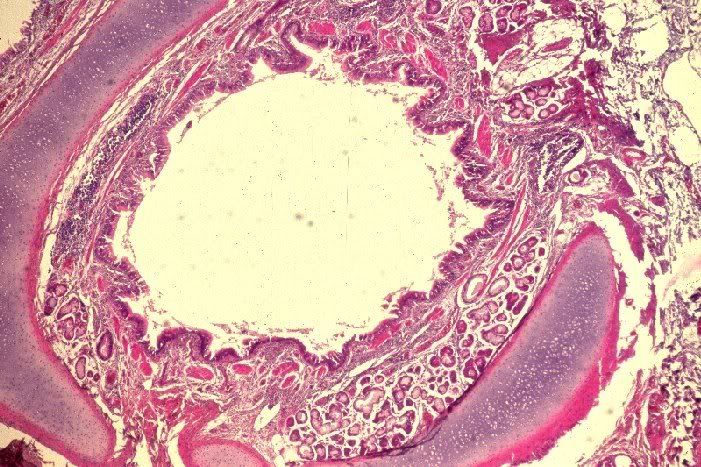
Figure 6: One of the bronchi. (From http://umanitoba.ca/faculties/medicine/units/anatomy/images/br22.JPG)
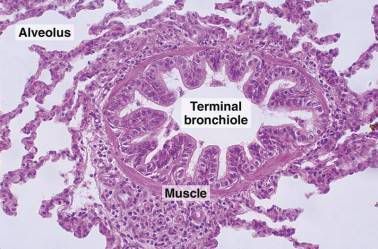
Figure 7: A terminal bronchiole. (From http://www.mc.vanderbilt.edu/histology/labmanual2002/labsection2/Respiratory03_files/image008.jpg)
Larger bronchioles have typical respiratory epithelium-- ciliated pseudostratified columnar epithelium [7]. As the bronchioles decrease in size, the epithelium transitions to ciliated cuboidal cells. Terminal bronchioles contain this ciliated simple cuboidal epithelium and have a thin lamina propria with elastic fibers and smooth muscle cells [1, 8]. They also contain Clara cells which are cilia free dome shaped cells present in the epithelium [8]. They secrete proteins which may assist the bronchi with protection from inflammation. The terminal bronchioles transition into the respiratory bronchioles, which are the first structures which belong to the respiratory portion of the respiratory system. They branch into several alveolar ducts which then lead to the alveoli [1, 8].
The Alveoli
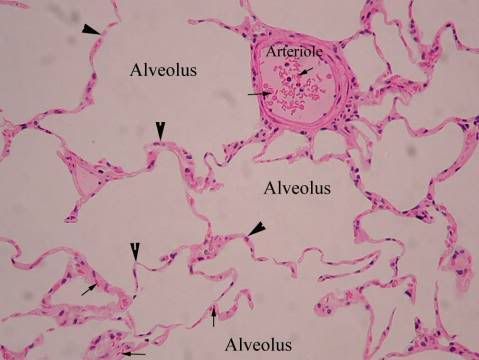
Figure 8: The alveoli (From http://www.octc.kctcs.edu/GCaplan/anat2/notes/image002.jpg)
Alveolar walls (or interalveolar septa) are composed of a thin squamous layer of epithelial cells and a small amounts of collagen, reticular and elastic fibres [1, 8]. Between the septa (in an area known as the interstitium) there is a dense network of pulmonary capillaries which are in direct contact with the epithelium of the alveoli. It is here that gas exchange between the lungs and the blood occurs [1, 2].
The epithelium of the alveoli is composed of two types of cells:
1. Alveolar type I cells. These cells are squamous and can be as thin as 0.05 um. They form 95% of the bulk of the alveolar epithelial surface [2, 8].
2. Alveolar type II cells. These cells are irregular of cuboidal shaped and form small bulges on the alveolar walls. Their cytoplasm contains a large number of granules (called cytosomes) which secrete the precursors of pulmonary surfactant. Surfactant is a mixture of proteins and phospholipids which reduce the surface tension of the alveoli, and prevent their collapse during exhalation, and act as a bactericide [2, 8].
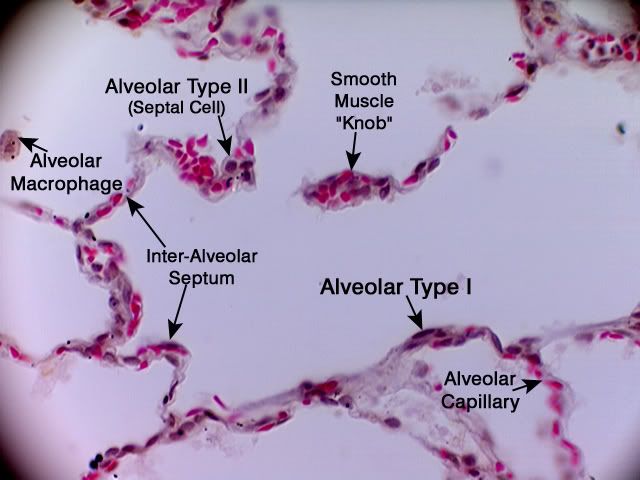
Figure 10: Type I and type II alveolar cells, the interalveolar septum, and the alveolar macrophages. (From http://www.octc.kctcs.edu/GCaplan/anat2/notes/A83_Alveoli_TypeI&II_40X.jpg)
There are no cilia present on the alveolar epithelium and thus no debris which is inhaled can be removed in this fashion [2]. However,another type of cell-- the alveolar macrophage-- migrate freely over the epithelium and ingest any inhaled debris which has escaped the mucus and cilia of the conducting airways [1, 8]. At the end of their lifespan they migrate to the bronchioles and enter the mucus lining to be discharged into the pharynx and swallowed [8].
The alveolar-capillary barrier, which refers to the structures oxygen and carbon dioxide must cross to be exchanged, prevents air bubbles from forming in the blood and prevents blood from entering the lungs. It includes pulmonary surfactant, the alveolar type I cells, the endothelial cells of the capillaries, and the basement membrane between the two [1, 2, 8].